Pain Anti Inflammatory Guide: Expert Insights for 2026
The landscape of pain management is evolving rapidly as science, technology, and natural therapies come together to offer new hope for those seeking relief. Chronic pain is a widespread challenge, but recent pain anti inflammatory breakthroughs are reshaping how we approach comfort and healing.
This comprehensive 2026 guide delivers expert insights into the science of inflammation, explores both conventional and next-generation treatments, and highlights holistic strategies for lasting relief. Discover proven pain anti inflammatory solutions, expert tips, and actionable advice to help you regain mobility and improve your quality of life.
Use this guide to make confident, informed choices and take control of your journey toward a pain-free, healthier future.
Understanding Inflammation and Pain: The Science Explained
Understanding the science behind pain anti inflammatory strategies begins with inflammation itself. Inflammation is a natural process, but when it persists, it can drive pain and disease. To manage pain anti inflammatory approaches effectively, it is crucial to recognize how inflammation operates in the body.
What is Inflammation? Acute vs. Chronic Pain
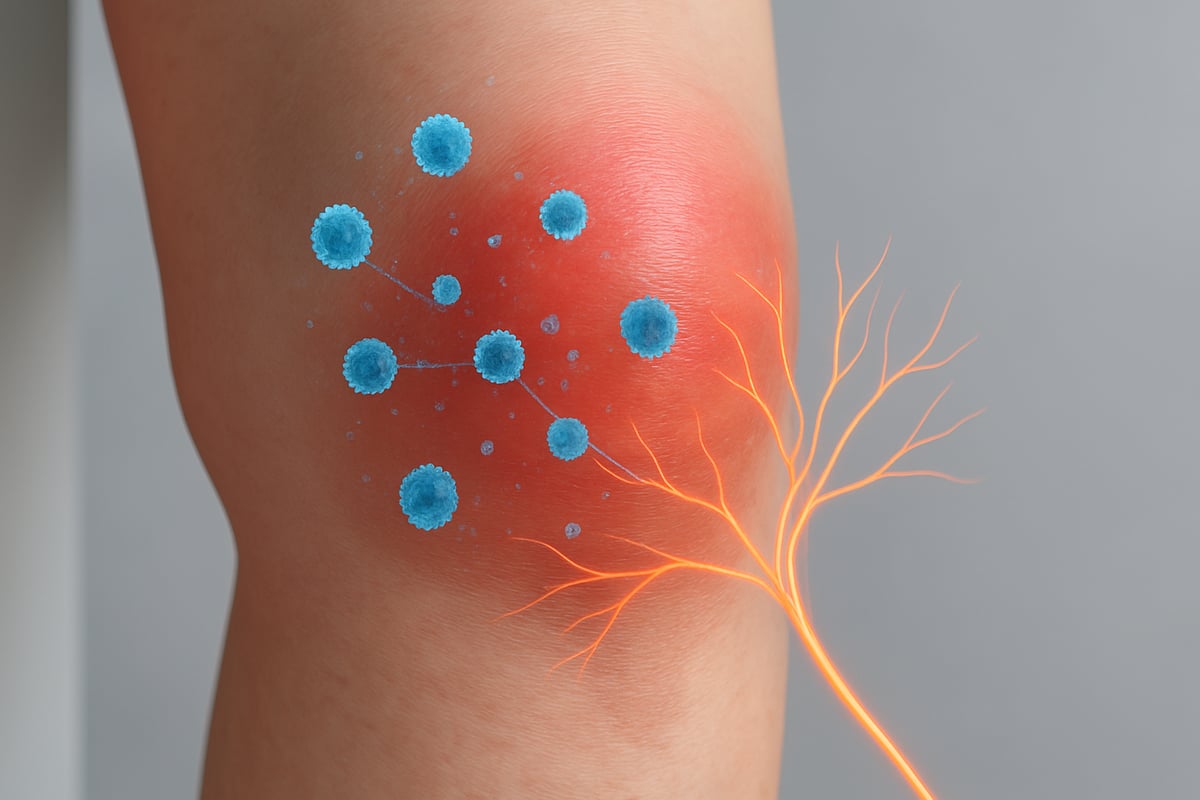
Inflammation is the body's frontline defense against injury or infection. In acute cases, such as a sprained ankle, the immune system triggers swelling, redness, and heat to repair tissue. This kind of inflammation is short-lived and resolves as healing occurs.
Chronic inflammation, however, is different. It lingers for months or years, even when there is no immediate threat. Conditions like rheumatoid arthritis or lupus are prime examples, where the immune system mistakenly attacks healthy tissue. This persistent response often leads to ongoing pain anti inflammatory needs.
The key difference lies in duration and purpose:
- Acute inflammation: Quick, protective, and resolves after healing.
- Chronic inflammation: Prolonged, can damage organs and joints, often underlies pain anti inflammatory treatment plans.
Recognizing these forms helps shape effective pain anti inflammatory interventions.
Biochemical Pathways of Pain and Inflammation
At the molecular level, pain anti inflammatory responses are shaped by complex biochemical signals. Cytokines, such as IL-1a, IL-1b, IL-6, and TNF-α, play central roles by amplifying inflammation and directly causing pain.
The arachidonic acid cascade is another crucial pathway. When tissue is damaged, enzymes like COX-1, COX-2, and LOX convert arachidonic acid into prostaglandins, thromboxanes, and leukotrienes. These mediators increase blood flow, sensitize nerves, and recruit immune cells.
| Enzyme | Main Product | Effect on Pain/Inflammation |
|---|---|---|
| COX-1 | Prostaglandins | Maintains gut lining, can cause pain |
| COX-2 | Prostaglandins | Drives inflammation and pain |
| LOX | Leukotrienes | Promotes immune cell migration |
Medications like NSAIDs target COX enzymes, reducing prostaglandin production and offering pain anti inflammatory relief (see Figure 1). Recent research, including the Effects of Natural Compounds on Inflammatory Pain, highlights how certain plant-derived compounds can also regulate these pathways and microglial activation, expanding pain anti inflammatory options beyond pharmaceuticals.
How Inflammation Causes Pain
Inflammation triggers pain anti inflammatory reactions through several mechanisms:
- Tissue swelling: Increased fluid puts pressure on nerves.
- Nerve sensitization: Chemicals like prostaglandins lower the pain threshold, making nerves more responsive.
- Immune cell recruitment: White blood cells release substances that can damage tissue or heighten pain.
If inflammation is not controlled, it can transition into chronic pain syndromes. This is common in disorders like fibromyalgia or osteoarthritis, where pain anti inflammatory solutions become lifelong needs.
Statistics show that over 50 million Americans live with inflammatory pain conditions. This prevalence highlights the urgent need for improved pain anti inflammatory strategies and awareness.
Key Takeaways
Gaining a clear understanding of inflammation is the foundation for effective pain anti inflammatory management. Acute and chronic inflammation differ profoundly, influencing how pain anti inflammatory treatments are chosen.
Ignoring chronic inflammation can lead to persistent pain, joint deterioration, and broader health risks. Early intervention, accurate diagnosis, and targeted pain anti inflammatory therapies are essential for long-term well-being.
By staying informed about the science, individuals and healthcare providers can make better decisions and leverage the latest pain anti inflammatory advances for optimal relief.
Conventional Anti-Inflammatory Treatments: Current Standards and Future Trends
Conventional pain anti inflammatory treatments have long formed the backbone of pain management. As science advances, understanding their mechanisms, benefits, and evolving risks becomes crucial for patients and providers alike. This section breaks down the current standards, emerging trends, and what the future may hold for pain anti inflammatory therapies.

NSAIDs: Mechanisms, Benefits, and Risks
Non-steroidal anti-inflammatory drugs (NSAIDs) are among the most widely used pain anti inflammatory medications worldwide. They work by inhibiting cyclooxygenase (COX-1 and COX-2) enzymes, which are crucial in the production of prostaglandins—chemicals that drive inflammation and pain.
Common NSAIDs include ibuprofen, naproxen, and aspirin. They provide rapid relief and are easily accessible over the counter, making them a first-line choice for many pain anti inflammatory needs.
However, NSAIDs are not without risk. Gastrointestinal upset, ulcers, and kidney issues can arise, especially with chronic use. In fact, up to 10 percent of kidney failures are associated with NSAID overuse. There are also concerns about delayed tissue healing and muscle regeneration when NSAIDs are used excessively. Figure 1 illustrates how NSAIDs block COX enzyme activity, highlighting their central role in pain anti inflammatory action.
Steroidal Anti-Inflammatories: Use and Limitations
Corticosteroids are another mainstay in pain anti inflammatory therapy. These medications mimic hormones produced by the adrenal glands and suppress multiple inflammatory pathways, offering potent relief for severe pain and autoimmune conditions.
Steroids are typically prescribed for short-term use due to their risk profile. Documented side effects can impact quality of life, especially with prolonged use:
| Side Effect | Frequency |
|---|---|
| Weight gain | Common |
| Mood changes | Common |
| Osteoporosis | Moderate |
| Adrenal suppression | Moderate |
Short-term corticosteroid use is often tolerated, but long-term therapy increases the likelihood of complications. Patients on chronic steroid regimens for pain anti inflammatory management must be closely monitored to avoid these adverse outcomes. Collaboration with healthcare providers is essential to balance benefits with potential harms.
Selective COX-2 Inhibitors: Evolution and Controversies
Selective COX-2 inhibitors were developed to minimize the gastrointestinal side effects common with traditional NSAIDs. Medications like celecoxib (Celebrex), rofecoxib (Vioxx), and valdecoxib (Bextra) offered targeted pain anti inflammatory action by selectively blocking the COX-2 enzyme.
Initially, these drugs gained rapid adoption, with 15 to 20 million users in the US. However, concerns arose when studies revealed increased cardiovascular risks. The APPROVe study found that Vioxx doubled the risk of thromboembolic events, leading to its withdrawal from the market. The heightened risk is linked to unopposed thromboxane production, increasing clotting potential.
Despite these controversies, COX-2 inhibitors remain a valuable pain anti inflammatory option for certain patients, especially those at risk for GI complications, but require careful risk assessment.
Emerging Pharmaceutical Innovations
The landscape of pain anti inflammatory treatment is evolving rapidly. Next-generation NSAIDs and biologic therapies are in development, aiming to provide targeted relief with fewer side effects. Biologics, such as monoclonal antibodies, offer precision by blocking specific inflammatory cytokines involved in chronic pain.
Personalized medicine is also making strides, with pharmacogenomics allowing treatments tailored to an individual's genetic profile. Regulatory agencies are closely monitoring these advancements to ensure safety and efficacy as new drugs reach the market.
A recent breakthrough includes the FDA Approves First Non-Opioid Pain Drug in 20 Years, which highlights the ongoing search for innovative and safer pain anti inflammatory solutions. These advancements promise a future where pain anti inflammatory care is more effective, personalized, and sustainable.
Natural and Alternative Anti-Inflammatory Solutions
Natural and alternative approaches have become central to pain anti inflammatory care. As science advances, more people are seeking options beyond conventional medications. This section explores the most promising compounds, the rise of CBD, and integrative therapies for holistic relief.

Popular Natural Compounds for Inflammation
Many individuals turn to natural compounds for pain anti inflammatory support. These options often target similar pathways as pharmaceuticals, but may offer fewer side effects.
Common Natural Compounds and Their Actions
| Compound | Mechanism | Evidence Level | Key Benefit |
|---|---|---|---|
| Turmeric/Curcumin | COX-2, NF-kB inhibition | Strong | Joint pain, arthritis |
| Omega-3 Fatty Acids | Prostaglandin modulation | Moderate | Joint health, inflammation |
| Ginger | Anti-inflammatory phenols | Moderate | Muscle soreness |
| Boswellia serrata | Leukotriene inhibition | Moderate | Arthritis relief |
| Bromelain | Proteolytic enzyme action | Emerging | Swelling, post-injury |
Turmeric’s curcumin content has shown promise in reducing inflammation through COX-2 and NF-kB suppression. Omega-3 fatty acids, found in fatty fish, help balance inflammatory prostaglandins. Ginger contains bioactive phenols that ease muscle soreness and joint discomfort.
Boswellia serrata, used in traditional medicine, works by blocking leukotrienes, making it useful for chronic pain anti inflammatory needs. Bromelain, an enzyme from pineapple, is valued for managing swelling after injury.
Safety is essential. While most natural compounds are well-tolerated, they can interact with medications or cause side effects like gastrointestinal upset. Consulting healthcare providers before starting any new pain anti inflammatory regimen is crucial.
The Role of CBD and Hemp-Based Products in Pain Management
CBD and hemp-based products have rapidly gained attention for pain anti inflammatory applications. These compounds interact with the body’s endocannabinoid system, which helps regulate inflammation and pain signals.
CBD modulates cytokine production, potentially reducing inflammatory responses in arthritis, neuropathic pain, and fibromyalgia. Recent studies point to significant improvements in pain and function among users of high-quality CBD oils and topicals.
Legal status is evolving, with most states allowing hemp-derived CBD under strict quality controls. Product transparency, including third-party lab testing, ensures purity and potency. It is important to choose reputable brands and check for certificates of analysis.
For a deeper dive into how CBD supports pain anti inflammatory goals and the science behind its effects, see Can CBD Help Inflammation.
Patients often report fewer side effects compared to traditional medications, but some may experience drowsiness, dry mouth, or medication interactions. Always consult a healthcare provider before combining CBD with other treatments.
Integrative and Mind-Body Therapies
A comprehensive pain anti inflammatory plan often includes integrative therapies. These approaches address both the physical and psychological aspects of pain.
Therapies with Evidence for Inflammation Reduction:
- Acupuncture: May lower inflammatory markers and improve pain.
- Massage therapy: Eases muscle tension and supports circulation.
- Physical therapy: Promotes joint mobility and functional recovery.
Mind-body practices such as mindfulness meditation, yoga, and stress management techniques can reduce inflammatory cytokines and enhance overall well-being. Nutrition also plays a key role. Diets like the Mediterranean or plant-based approaches are rich in antioxidants and polyphenols, supporting pain anti inflammatory goals.
Regular exercise, even low-impact activities like swimming or walking, helps control systemic inflammation and supports healing. Integrating these therapies creates a balanced, sustainable plan for lasting relief.
Lifestyle Strategies for Lasting Pain and Inflammation Control
Making lasting changes to your daily habits is essential for effective pain anti inflammatory management. By focusing on nutrition, movement, sleep, and behavior, you can significantly reduce inflammation and boost overall well-being. Explore the most effective strategies below for a holistic approach to pain anti inflammatory relief.

Diet and Nutrition for Inflammation
Your diet is a powerful tool for pain anti inflammatory control. Choose foods rich in antioxidants and healthy fats to help your body fight inflammation naturally.
- Anti-inflammatory foods: Fatty fish like salmon, sardines, and mackerel provide omega-3s that calm inflammation. Add berries, leafy greens, nuts, and olive oil for a nutrient boost.
- Foods to avoid: Processed meats, sugary drinks, and refined carbohydrates can trigger inflammatory pathways.
- Antioxidants and polyphenols: Colorful fruits and vegetables are packed with compounds that neutralize free radicals.
For a comprehensive overview of natural strategies, visit Pain Relief Natural Methods to discover additional insights on diet and holistic pain anti inflammatory approaches.
Physical Activity and Movement
Regular movement is one of the most effective pain anti inflammatory tactics. Exercise helps decrease systemic inflammation and improves healing, even for those with chronic pain.
- Safe options: Yoga, swimming, and walking are gentle on joints and support flexibility.
- Physical therapy: Tailored exercise routines can address specific pain areas and prevent further injury.
- Movement modification: Learn proper techniques to minimize strain and maximize benefit.
Consistency is key. Start slow, listen to your body, and gradually increase intensity as tolerated.
Sleep, Stress, and Recovery
Poor sleep can worsen inflammation and undermine pain anti inflammatory efforts. Prioritizing restorative rest and stress management is vital.
- Sleep hygiene: Maintain a regular sleep schedule, create a calming bedtime routine, and limit screen time before bed.
- Stress reduction: Mindfulness, meditation, and cognitive behavioral therapy can lower inflammatory cytokine levels.
- Relaxation techniques: Deep breathing and gentle stretching before bed may improve sleep quality.
Aim for seven to nine hours of quality sleep each night to support recovery and reduce pain.
Environmental and Behavioral Modifications
Simple changes in your environment and habits can make a big difference in pain anti inflammatory outcomes.
- Ergonomics: Adjust your workspace and home setup to minimize joint strain.
- Lifestyle choices: Quit smoking, limit alcohol, and work toward a healthy weight.
- Behavioral habits: Use supportive shoes, take breaks from repetitive tasks, and maintain good posture.
These practical adjustments, when combined with nutrition, movement, and stress management, create a strong foundation for lasting pain relief and inflammation control.
The Future of Anti-Inflammatory Pain Management: Expert Predictions for 2026
The landscape of pain anti inflammatory care is rapidly evolving, with science and technology reshaping what relief means for millions. As we look toward 2026, innovative treatments, digital tools, and patient-centered approaches are converging to redefine standards of care. Let us explore the most promising directions experts predict for the future of pain anti inflammatory management.
Advances in Biologic Therapies and Personalized Medicine
Personalized medicine is transforming pain anti inflammatory strategies by targeting inflammation at the molecular level. Biologic drugs, such as monoclonal antibodies, are designed to block specific cytokines like TNF-α and IL-6, offering tailored relief for conditions like rheumatoid arthritis. Gene therapies are also emerging, aiming to modify the body's inflammatory response for lasting results.
Pharmacogenomics is enabling clinicians to match patients with the most effective pain anti inflammatory treatments based on their genetic profile. This approach reduces trial and error, improving outcomes and minimizing side effects. As these therapies become more accessible, the future holds the promise of highly individualized care.
Digital Health and Remote Monitoring
Digital health technologies are set to play a pivotal role in pain anti inflammatory management. Wearable devices now allow patients to monitor inflammation markers, pain levels, and activity in real time. Data collected from these devices can be shared instantly with healthcare providers, enabling faster interventions and more precise adjustments to treatment plans.
AI-driven apps are also supporting patients with chronic pain through tailored education, symptom tracking, and virtual consultations. Innovative online interventions, such as Personal Danger Signals Reprocessing for Chronic Pain, are expanding access to non-pharmacological therapies and empowering individuals to take control of their pain anti inflammatory journey.
Integrative Care Models
The future of pain anti inflammatory care is increasingly collaborative. Multidisciplinary pain clinics are bringing together physicians, physical therapists, nutritionists, and alternative practitioners to design comprehensive, integrative plans. This team-based approach ensures that medical, physical, and emotional needs are addressed in tandem.
Insurance providers are beginning to recognize the value of integrative therapies, expanding coverage for acupuncture, massage, and even select natural interventions. As new research supports the efficacy of alternatives like cannabinoids, patients may benefit from options such as Exploring the Potential of CBD-Based Alternatives to Steroid Medications, offering a holistic approach to pain anti inflammatory relief.
Patient Empowerment and Education
Empowering patients is a cornerstone of effective pain anti inflammatory care. Access to reliable, up-to-date information is essential for making informed choices. Shared decision-making models are gaining traction, encouraging open dialogue between patients and providers.
Peer support networks, digital communities, and educational resources are helping individuals become active participants in their pain anti inflammatory management. By fostering self-advocacy, patients are better equipped to navigate complex treatment landscapes and sustain long-term wellness.
Challenges and Ethical Considerations
With rapid innovation in pain anti inflammatory therapies, new challenges emerge. Balancing the safety, efficacy, and affordability of advanced treatments is a pressing concern. Health disparities persist, making equitable access to cutting-edge care a priority for policymakers and providers.
Ongoing research and regulatory oversight remain crucial to ensure that novel pain anti inflammatory solutions are both effective and safe. The future will demand ethical frameworks to guide the responsible adoption of these transformative therapies.
Expert Tips and Actionable Steps for Managing Pain and Inflammation
Effectively managing pain anti inflammatory challenges requires a strategic, evidence-based approach. By following these expert steps, you can take control of your health, reduce discomfort, and promote long-term wellness.
Step 1: Get a Comprehensive Diagnosis
Begin your pain anti inflammatory journey by seeking a thorough evaluation. Accurate diagnosis is essential to identify the root causes of inflammation and pain.
Healthcare providers may recommend imaging, blood tests, and specialist consultations. This helps distinguish between acute and chronic issues, ensuring targeted treatment.
- Ask about inflammatory markers in bloodwork.
- Document your symptoms in detail.
- Request referrals to rheumatologists or pain specialists if needed.
A comprehensive diagnosis lays the groundwork for effective, individualized care.
Step 2: Build a Personalized Anti-Inflammatory Plan
Work with your medical team to develop a tailored pain anti inflammatory strategy. This plan should integrate medications, natural therapies, and lifestyle adjustments.
Explore options such as physical therapy, dietary changes, and evidence-based supplements. For those interested in alternatives, consider reviewing How CBD Can Help With Arthritis for insights on CBD's role in inflammation and pain.
Regularly revisit your treatment plan to ensure it evolves with your needs.
Step 3: Monitor Progress and Adjust Strategies
Track your pain anti inflammatory progress using tools like pain diaries, symptom trackers, or wearable technology. Monitoring allows you to spot patterns, recognize triggers, and address side effects early.
- Note pain intensity and frequency daily.
- Share updates with your healthcare provider.
- Adjust treatment based on response and flare-ups.
Consistent monitoring empowers you to make informed decisions and optimize outcomes.
Step 4: Prioritize Education and Self-Advocacy
Stay informed about pain anti inflammatory research and emerging therapies. Accessing trusted resources helps you understand new developments and make confident choices.
Engage in patient communities, seek second opinions, and read up on topics like Estrogen's Role in Natural Pain Relief to broaden your understanding of pain mechanisms.
Self-advocacy is key to ensuring your voice is heard in every stage of your care.
Step 5: Focus on Long-Term Wellness
Sustainable pain anti inflammatory management means setting realistic goals and maintaining healthy habits. Incorporate regular exercise, restorative sleep, and balanced nutrition to support healing.
Lean on support networks for motivation and accountability. Celebrate progress, however small, and remain proactive about your well-being.
With dedication and expert guidance, long-term relief is within reach.
As you’ve explored the latest expert insights and practical strategies for tackling inflammation and chronic pain, it’s clear that taking action today can make a real difference in your comfort and quality of life. Reclaim Labs is committed to supporting you on this journey by offering premium, thoroughly tested CBD hemp oil products designed for safe, effective relief. If you’re ready to put expert-backed solutions into practice and move toward lasting wellness, I encourage you to Get Relief Now! and discover natural options that put your health first.
